Difference between revisions of "DBP3:Utah:RegCases"
| Line 89: | Line 89: | ||
* We are currently defining an optimized set of registration parameters for each of the above cases | * We are currently defining an optimized set of registration parameters for each of the above cases | ||
| − | * A Slicer extension module has been developed and pre-defined registration parameters are being tuned for each of the above scenarios | + | * A [[DBP3:Utah:SlicerModuleCardiacRegistration | Slicer extension module]] has been developed and pre-defined registration parameters are being tuned for each of the above scenarios |
| − | * The module takes as input two | + | * The module takes as input two image volumes and a drop-down menu lets the user select the appropriate registration scenario |
* The module returns a registered output image | * The module returns a registered output image | ||
| + | * Advanced registration parameters can be adjusted in order to improve the registration output | ||
Revision as of 23:43, 15 November 2012
Home < DBP3:Utah:RegCasesBack to Utah AFib DBP
Background
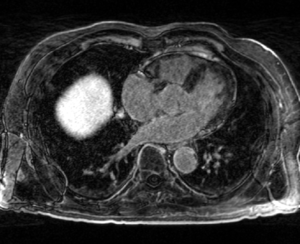
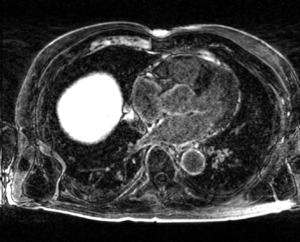
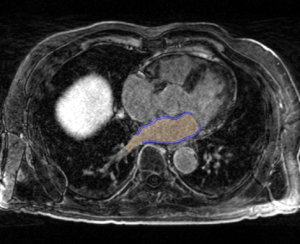
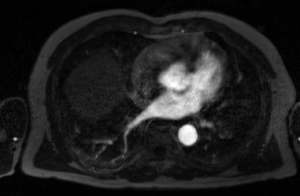
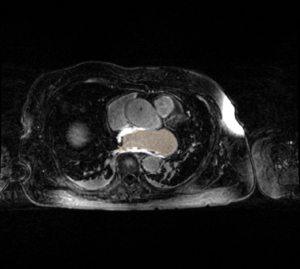
- The CARMA Center uses late gadolinium enhanced MRI (LGE-MRI) images to evaluate new patients, predict procedural success, and evaluate therapeutic outcomes. The MRI images for each patient are further accompanied by MR angiographic images (MRA) and manual segmentations of relevant structures. These images are acquired longitudinally over the course of a patient's evaluation, treatment, and follow-up (i.e. months or years). Registration is often necessary to compare images from different time points in a patient's treatment, different patients at the same stage of disease progression or treatment, and different image types. Registration is needed for a variety of combinations of common image types encountered at CARMA:
| Pre-ablation LGE-MRI Image | Post-ablation LGE-MRI Image | Segmentation of LGE-MRI Image |
|---|---|---|
| MRA Image | Immediately Post-ablation LGE-MRI Image | CT Image |
- Pre-ablation scans are acquired before the procedural. Bright portions in the LA wall is indicative of fibrosis; fibrosis scores are used to stratify and triage patients based on their Utah score.
- Post-ablation scans are acquired 3 months and later after the procedure. These scans have higher contrast (brighter regions) in the LA wall indicative of scaring from the ablation procedure.
- Segmentations will be binary label masks manually-contoured by experts at CARMA.
- MRAs have a bright blood pool, the bounds of which indicate the endocardial surface of the LA wall.
- Immediately-post ablation scans exhibit large, bright areas in and around the LA walls, reflecting edema and shape changes caused by the ablation procedures.
- CT scans are less common but can be acquired with a contrast agent to delineate the bounds of the blood pool. Many of our CT scans are acquired with a C-arm fluoroscopy unit rather than a traditional CT scanner.
Registration Case Types
These are current projects at CARMA which could be aided by improved, case-specific registration algorithms. The projects are sorted according to the types of images to be registered.
Pre to Post LGE-MRI
- Residual fibrosis project -- Nazem Akoum
Registration of pre to post (at least 3 months) LGE-MRI to examine the overlap of fibrosis and post-procedural scar. Findings may support targeting ablations to areas of intense fibrosis. Registration may be complicated as LA volume will decrease after ablation.
Pre to Pre LGE-MRI
- AF progression -- UMAC
Registration of images from animals with induced AF to examine the progression of the disease. There will be multiple time points for each animal; scans are often acquired monthly. Registration will allow for changes in shape, volume, and fibrosis distribution to be examined. We may also look at registering images across different animals.
- Longitudinal pre-ablation scans -- Nathan Burgon/Chris McGann
Similar to the UMAC AF progression study, examining the progression of AF in humans. Scans will all be longitudinal pre-ablation; these scans typically come from patients who opt not to be ablated. The time between scans will likely be irregular and possibly as much as a couple years.
Post to Post LGE-MRI
- Permanent scar formation -- Koji Higuchi
This study examines at lost 2 post-ablation scans (likely 3 months and 2 years post-ablation). This allows us to assess the permanence of scar after the blanking period (3 months) to more stable, long-term scar formation.
MRA to LGE-MRI
- MRA threshold-based segmentation -- Image processing group
The MRA captures the extent of the blood pool and roughly corresponds to the endocardial surface of the LA wall. The MRA is also much easier to automatically segment. Registration of the MRA to LGE-MRI would allow for segmentation of the MRA blood pool as an initial guess in segmentation of the LGE-MRI blood pool. We will likely need gated MRAs.
MRA to MRA
- Shape-analysis studies -- Image processing group
The MRA is a quick and dirty way of capturing the bounds of the blood pool for shape studies. Alignment of the MRAs will allow for alignment of the blood pool masks for input into shape analysis pipelines (i.e., ShapeWorks)
Immediately-Post to Post LGE-MRI
- Ablation gaps -- Ravi Ranjan
Registration of animal scans or patient scans to look for the appearance of gaps in the lesion sets after ablation and how that impacts scar development.
- No-reflow studies -- Chris McGann
A more general variation of the gap study; how do no-reflow regions spatially correlate to permanent scar formation. Challenges will include major inflammation, variable wall thickness, and deformation.
Vector-Valued Registration
- Cardiac-specific image registration -- Yi Gao/Josh Cates
A collaboration with Yi Gao et al. to use blood pool segmentation and raw images before and after ablation to more accurately register the cardiac anatomy from the images.
CT to LGE-MRI
- Shape-analysis studies -- Image processing group
CT better captures the shape of the LA and is more easily segmented. We hope to compare the volumes and shapes of CT-derived LA segmentations to those of MRI-segmented images. We will need to register the CT and MRI images to make this work. A potential challenge here is the scarcity of CT scans (namely normal CT scans, although, DynaCT scans are also not commonly acquired).
Implementation
- We are currently defining an optimized set of registration parameters for each of the above cases
- A Slicer extension module has been developed and pre-defined registration parameters are being tuned for each of the above scenarios
- The module takes as input two image volumes and a drop-down menu lets the user select the appropriate registration scenario
- The module returns a registered output image
- Advanced registration parameters can be adjusted in order to improve the registration output