|
|
| (56 intermediate revisions by 6 users not shown) |
| Line 1: |
Line 1: |
| − | * The Driving Biological Problem for NA-MIC at The MIND Institute: The Analysis of Brain Lesions in Neuropsychiatric Systemic Lupus Erythematosis
| + | Back to [[DBP2:Main|NA-MIC DBP 2]] |
| − | * co-PIs H Jeremy Bockholt and Charles Gasparovic
| + | __NOTOC__ |
| − | * The MIND Institute
| + | = Overview of MIND DBP 2 = |
| | + | == The Analysis of Brain Lesions in Neuropsychiatric Systemic Lupus Erythematosus == |
| | | | |
| − | * Research Goals
| + | Critical to understanding the etiology of brain lesions in NPSLE will be the accurate measurement of their location, size, and time course. Lupus brain lesions are known to vary in MRI intensity and temporal evolution and include acute, chronic, and resolving cases. Monitoring the time course of image intensity changes in the vicinity of lesions, therefore, may serve to classify them based on their temporal characteristics. Hence, a major objective of this DBP will be the evaluation of existing tools and the development new tools within SLICER for the time series analysis of brain lesions in lupus. [[DBP2:MIND:Introduction|More...]] |
| − | Systemic lupus erythematosus (SLE) is an autoimmune disease affecting multiple tissues, including the brain. Estimates of SLE prevalence range from 14.6-372 per 105 (1). Neuropsychiatric SLE (NPSLE), a term that subsumes the neurologic and psychiatric complications of SLE, occurs in up to 95% of SLE patients (2). While MRI often reveals distinct white matter abnormalities in active NPSLE, the pathologic processes underlying these lesions, whether purely autoimmune or vascular (e.g., hemostasis), are unknown.
| |
| | | | |
| − | Currently we are testing hypotheses concerning the possible thrombotic or embolic origin of white matter brain lesions in NPSLE and, ultimately, the cause of cognitive dysfunction in NPSLE. Specifically, we are examining whether the incidence of lesions correlates with either levels of thrombosis markers or emboli in the blood or a potential source of emboli in the heart. We will also examine whether overall lesion load or the levels of particular classes of lesion correlate with cognitive function. Diffusion-weighted, T1-weighted, and T2-weighted MRI are used to classify normal tissue and lesions. Additionally, blood flow is measured with perfusion-weighted imaging and vascular status is assessed with MR angiography.
| + | Data is provided at the following link: '''[[Data:DBP2:MIND|MIND Data]]'''. |
| | | | |
| − | Critical to understanding the etiology of brain lesions in NPSLE will be the accurate measurement of their location, size, and time course. Lupus brain lesions are known to vary in MRI intensity and temporal evolution and include acute, chronic, and resolving cases. Monitoring the time course of image intensity changes in the vicinity of lesions, therefore, may serve to classify them based on their temporal characteristics. Hence, a major objective of this DBP will be the evaluation of existing tools and the development new tools within SLICER for the time series analysis of brain lesions in lupus.
| + | = MIND Roadmap Project = |
| | | | |
| − | * Data
| + | {| cellpadding="10" border="1" style="background:lightblue;text-align:left;" |
| | | | |
| − | The MRI data in this project are collected on a 1.5T Siemens Sonata scanner using an 8-channel head coil. Whole-brain images to measure brain volume changes and identify lesions are obtained with three co-registered pulse sequences in an oblique-axial plane aligned with the interhemispheric midline and parallel to the anterior commissure-posterior commissure (AC-PC) line: 1) a T1-weighted 3D fast low angle shot (FLASH) sequence (TR/TE = 12/4.76ms, flip angle = 20deg, FOV = 220x220mm, resolution = 192x192, 120 1.5-mm slices, total time = 6m32s), 2) a T2-weighted fast spin echo sequence (TR/TE = 9040/64ms, turbofactor=5, FOV = 220x220mm, resolution = 192x192, 120 1.5-mm slices, total time = 6m2s) and 2) a Fluid Attenuated Inversion Recovery (FLAIR)/fast spin echo sequence (TR/TE = 1000/105ms, TI = 2500ms, echo train=9, field of view (FOV) = 220x220mm, resolution = 192x192, 88 1.5-mm slices, total time = 9m2s). We employ a perfusion-weighted EPI sequence to follow the first pass of a contrast bolus through the brain (TR/TE = 2120ms/65ms, flip angle = 90º, 20 5-mm slices, a time course of 60 sequential acquisitions, FOV=220x220 mm, matrix size 128x128). From the signal intensity curve calculated over the time series, relative cerebral blood flow, relative cerebral blood volume, and relative mean transit time are calculated. MR angiography is performed with a region of interest centered on the circle of Willis using a 3D FLASH-based time-of-flight sequence (TR/TE = 40ms/7.15ms, flip angle = 25º, FOV=200x200 mm, matrix size 256x256, 128 0.8-mm slices, scan time=6m27s)
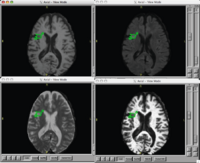
| + | | style="width:15%" | [[Image:Lupus.png|200px]] |
| | + | | style="width:85%" | |
| | | | |
| − | In addition to MRI, transcranial doppler ultrasound is used to detect microemboli in the brain and transesophageal echocardiography is performed to evaluate general cardiac status and to detect the presence of heart valve vegetations, as potential sources of emboli. A number of laboratory tests on blood samples are performed to detect markers of hemostasis, including analyses for platelets, coagulation, fibrinolysis, and anti-phospholipid antibodies. Finally, a battery of neuropsychological tests is administered to evaluate cognitive function. These exams, along with the MRI, will be performed on approximately 60 SLE patients and 30 normal control subjects over a period of 48 months. A subset of this group will be approximately 15 SLE subjects with NPSLE and 15 SLE subjects without NSLE who are recruited and examined during the first year of the study. A subset of these initial SLE groups will be re-examined in the each of the subsequent years (2-4) of the study.
| + | == [[DBP2:MIND:Roadmap|Brain Lesion Analysis in Neuropsychiatric Systemic Lupus Erythematosus]] == |
| | | | |
| − | * Image Processing Needs
| + | Our goal is to automatically, or with little or no manual human rater input, accurately tissue classify our example lupus data-set into gray, white, csf, and lesion classes. [[DBP2:MIND:Roadmap|More...]] |
| − | Our major image processing needs in this project revolve around lesion segmentation and time series analysis. Hence, we need a robust and reliable method capable of segmenting the brain into at least four classes: gray matter, white matter, cerebrospinal fluid, and white matter lesions. Furthermore, in order to follow changes in lesions with time, and to allow the possibility of sub-classifying lesions according to their temporal features, we will need methods of normalizing and registering images obtained in different scanning sessions. Ultimately, such tools will allow us to ask questions such as whether the appearance of and changes in particular lesions correlate with the onset and remission of the neuro-psychiatric symptoms of NPSLE. | |
| | | | |
| − | A goal of the project will be to make this analysis fully automated. The input data will be image data from the T1-weighted, T2-weighted, and FLAIR sequences described above. Output data will be probability maps for each tissue class, the number of lesions, the volume of each lesion, and the total lesion volume at each time point. Additionally, changes in lesion size and changes in pixel intensity within the volume of each lesion will be displayed graphically. The time course data will also be amenable to time series analysis by statistical tools such as general linear modeling (GLM), independent component analysis (ICA), and Bayesian analysis.
| + | |} |
| − | | |
| − | | |
| − | * Current Image Processing Tools
| |
| − | Presently at the MIND Institute, a number of different MRI data analysis tools are used by researchers. These include modules in BRAINS2, FSL, SPM, Freesurfer, and Slicer for image segmentation and labeling and FSL, SPM, and AFNI for fMRI data analysis. The tissue classifying modules in these tools where developed for the segmentation of normal appearing tissue and none - except perhaps for Slicer recently - has been shown to be useful for lesion analysis. While other software tools are commercially available for lesion analysis of image data (e.g., Analyze), they are generally expensive and cross-validation studies on their performance are lacking.
| |
| − | | |
| − | * What We Will Do with the NA-MIC Kit
| |
| − | We will implement a novel best practice automated lesion segmentation algorithm that takes advantage of the strengths of existing algorithms and is implemented using the ITK framework. We will develop a module for Slicer that quantifies various lesion parameters and performs time series analyses on these parameters. A software engineer will be hired to implement these modules within Slicer, supervised jointly by Chuck Gasparovic and H. Jeremy Bockholt at the MIND Instutute. Vincent Magnotta, a tissue segmentation expert at the University of Iowa, and Wilber Sibbitt, the co-PI of the NPSLE project will act as consultants on the project.
| |
| − | | |
| − | More specifically, this project will proceed in three phases:
| |
| − | | |
| − | 1. We will evaluate the performance of at least four methods for lesion segmentation on a set of brain images: 1) a method using Slicer, developed by Sandy Wells, 2) a modification of this method involving pre-processing steps, developed by Vincent Magnotta, 3) a method using BRAINS2, and 4) manual classification by an expert rater. If warranted, other algorithms will be evaluated. We will use the STAPLE (3) and/or a method using the Williams Index (3) to cross-validate these methods.
| |
| − | 2. We will implement within Slicer methods for the registration and normalization of MRI images obtained in different scanning sessions, allowing the time series analysis of the data on a pixel-by-pixel basis.
| |
| − | 3. We will experiment with different statistical methods of time series analysis of these data, drawing from methods that have been successful in the analysis of fMRI data, including GLM and ICA. For example, we will experiment with the use of GLM or multiple regression analysis to examine correlations between changes in lesion intensity or size and measures of thrombo-embolic activity or the onset of clinical symptoms of NPSLE, as described above. If any of these methods proves useful in the analysis of the NPSLE data set, we will consider applying for external funds to implement them within the Slicer framework in a future project.
| |
| − | | |
| − | * Direction that this DBP Will Drive NA-MIC
| |
| − | The successful implementation of the methods developed in this DBP will have a broad impact on the study of brain diseases involving MRI-visible lesions. The origin of these lesions in many diseases - including NPSLE, vascular dementia, and multiple sclerosis - is still unknown. Moreover, it is not clear in many cases whether there are multiple causes for lesions, even within one subject (e.g., both autoimmune and embolic). The accurate characterization of the time evolution of these lesions, therefore, will undoubtedly help to elucidate not only the origins of the lesions but their relationships to disease symptoms. No image analysis software package currently permits this level of lesion analysis. Hence, the availability of these tools within Slicer will give it a unique position among software for brain lesion analysis.
| |
| − | | |
| − | * Summary
| |
| − | We will augment, develop, and validate tools within Slicer for the quantification of brain lesions thought to underlie the cognitive dysfunction of NPSLE. Furthermore, we will develop tools to analyze changes in these lesions with time and to relate these changes to the fluctuating symptoms of NPSLE. Our primary goal in the work, of course, is to gain greater insight into the causes of NPSLE. However, if successful, we will apply these tools to other brain diseases currently under investigation at UNM and The MIND Institute, including vascular dementia, myotonic dystrophy, and multiple sclerosis.
| |
| − | | |
| − | * References
| |
| − | 1. Aladjem, H (Editor): LFA study shows between 1,400,000 and 2,000,000 people diagnosed with lupus. Lupus News 14:12, 1994.
| |
| − | | |
| − | 2. Sibbitt WL Jr, Brandt JR, Johnson CR, Maldonado ME, Patel SR, Ford CC, Bankhurst, AD, BrooksWM: The incidence and prevalence of neuropsychiatric syndromes in pediatric-onset systemic lupus erythematosus. J Rheum 2002 29:1536-42.
| |
| − | | |
| − | 3. Warfield SK, Zou KH, Wells WM. Simultaneous truth and performance level estimation (STAPLE): an algorithm for the validation of image segmentation. IEEE Trans Med Imaging. 2004 Jul;23(7):903-21.
| |
| − | | |
| − | 4. Martin-Fernandez M, Bouix S, Ungar L, McCarley RW, Shenton ME. Two methods for validating brain tissue classifiers. Med Image Comput Comput Assist Interv Int Conf Med Image Comput Comput Assist Interv. 2005;8(Pt 1):515-22.
| |