Difference between revisions of "2017 Winter Project Week/3DSurgicalPlanningBreastReconstruction"
| Line 3: | Line 3: | ||
Image:PW-Winter2017.png|link=2017_Winter_Project_Week#Projects|[[2017_Winter_Project_Week#Projects|Projects List]] | Image:PW-Winter2017.png|link=2017_Winter_Project_Week#Projects|[[2017_Winter_Project_Week#Projects|Projects List]] | ||
<!-- Use the "Upload file" link on the left and then add a line to this list like "File:MyAlgorithmScreenshot.png" --> | <!-- Use the "Upload file" link on the left and then add a line to this list like "File:MyAlgorithmScreenshot.png" --> | ||
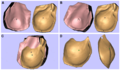
| + | Image:Chae2015-Fig4.png | ||
</gallery> | </gallery> | ||
Revision as of 18:56, 9 January 2017
Home < 2017 Winter Project Week < 3DSurgicalPlanningBreastReconstructionKey Investigators
- Michael Chae (Monash University, Australia)
- Andras Lasso (Queen’s University, Canada)
- Julian Smith (Monash University, Australia)
- Warren Rozen (Monash University, Australia)
- David Hunter-Smith (Monash University, Australia)
Project Description
| Objective | Approach and Plan | Progress and Next Steps |
|---|---|---|
|
|
|
Background and References
1 in 8 women in the US will be diagnosed with breast cancer in their lifetime. As genetic testing for breast cancer, such as BRCA1/2, becomes more available, an increasing number of women will be diagnosed early and evidences show that more and more women are opting for aggressive surgery (i.e. mastectomy) early on to achieve cure. As a result, post-mastectomy breast reconstruction has become an important component of the holistic treatment of patients with breast cancer. Breast reconstruction with autologous tissue (i.e. one’s own tissue) bypasses risks associated with traditional implants and provides a stable, natural-appearing, long-term volume replacement. The most ideal source of tissue for breast reconstruction is the abdominal wall. These tissues are raised as a free flap tissue based on small vessels, called perforators. Unfortunately, there is a significant variance in perforator size and locations between individuals. Advancements in modern imaging technologies, such as computed tomographic angiography (CTA), has enabled surgeons to select the appropriate perforator and facilitate flap design, leading to improvements in clinical outcomes. However, their efficacy is limited by being displayed on a two-dimensional (2D) surface. In contrast, imaging-guided 3D-printed surgical planning solution can provide tactile feedback and a superior appreciation of visuospatial relationship between anatomical structures. (1-4)
- [Chae2014] Chae, M. P., Hunter-Smith, D. J., Spychal, R. T., Rozen, W. M. 3D volumetric analysis for planning breast reconstructive surgery. Breast Cancer Res Treat 2014;146:457-460.
- Rozen, W. M., Phillips, T. J., Ashton, M. W., Stella, D. L., Gibson, R. N., Taylor, G. I. Preoperative imaging for DIEA perforator flaps: a comparative study of computed tomographic angiography and Doppler ultrasound. Plast Reconstr Surg 2008;121:9-16.
- Masia, J., Clavero, J. A., Larranaga, J. R., Alomar, X., Pons, G., Serret, P. Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg 2006;59:594-599.
- Chae, M. P., Rozen, W. M., McMenamin, P. G., Findlay, M. W., Spychal, R. T., Hunter-Smith, D. J. Emerging Applications of Bedside 3D Printing in Plastic Surgery. Front Surg 2015;2:25.
- Gerstle, T. L., Ibrahim, A. M., Kim, P. S., Lee, B. T., Lin, S. J. A plastic surgery application in evolution: three-dimensional printing. Plast Reconstr Surg 2014;133:446-451.